The Society of Surgical Oncology (SSO) and American Society for Radiation Oncology (ASTRO) formed a multidisciplinary expert panel in 2013 to examine the relationship between surgical margin width and ipsilateral breast tumor recurrence and develop guidelines on margins for breast-conserving surgery with whole-breast irradiation in stage I and II invasive breast cancer. The panel used a meta-analysis of margin width and ipsilateral recurrence from a systematic review of 33 studies published between 1965 and January 2013 including 28,162 patients as the primary evidence base for consensus.
The SSO-ASTRO guideline was published in Annals of Surgical Oncology, International Journal of Radiation Oncology*Biology*Physics, and Journal of Clinical Oncology1 and is available at www.surgonc.org/margins-study, www.redjournal.org, and jco.ascopubs.org.
Primary Clinical Question
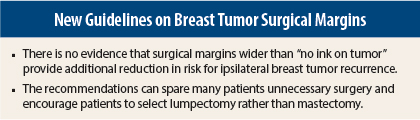
The primary clinical question the panel sought to answer was: What margin width minimizes the risk of ipsilateral breast tumor recurrence? Review of the evidence did not support routine removal of larger amounts of healthy breast tissue beyond having no cancerous cells touching the edge of the lumpectomy specimen, with this finding being true irrespective of patient age or presence of more aggressive, triple-negative cancer types. The panel hopes that the recommendations will spare many patients unnecessary surgery and encourage patients to select lumpectomy rather than mastectomy when medically appropriate.
Monica Morrow, MD, of Memorial Sloan Kettering Cancer Center and SSO, and Meena S. Moran, MD, of Yale University and ASTRO, were panel Co-Chairs. Nehmat Houssami, MD, PhD, of University of Sydney School of Public Health, performed the systematic review. The guideline was produced with a grant from Susan G. Komen and is endorsed by ASCO and the American Society of Breast Surgeons.
The clinical questions addressed by the panel and the resulting recommendations, along with level of evidence for each recommendation, are provided below.
Guidelines Summary
What is the absolute increase in risk of ipsilateral breast tumor recurrence with a positive margin? Can the use of radiation boost, systemic therapy, or favorable tumor biology mitigate this increased risk?
Recommendation: Positive margins, defined as ink on invasive cancer or ductal carcinoma in situ, are associated with at least a twofold increase in ipsilateral breast tumor recurrence. This increased risk in ipsilateral recurrence is not removed by delivery of a radiation boost, systemic therapy (endocrine therapy, chemotherapy, biologic therapy), or favorable biology. (Level of evidence: meta-analysis and secondary data from prospective trials and retrospective studies.)
Do margin widths wider than “no ink on tumor cells” reduce the risk of ipsilateral breast tumor recurrence?
Recommendation: Negative margins (no ink on tumor) optimize ipsilateral breast tumor recurrence. Wider margin widths do not significantly lower this risk. The routine practice of obtaining wider negative margin widths is not indicated. (Level of evidence: meta-analysis and retrospective studies.)
What are the effects of endocrine or biologically targeted therapy or systemic chemotherapy on ipsilateral breast tumor recurrence? Should a patient who is not receiving any systemic treatment have wider margin widths?
Recommendation: Rates of ipsilateral breast tumor recurrence are reduced with the use of systemic therapy. In the rare circumstance of a patient not receiving adjuvant systemic therapy, there is no evidence suggesting that margins wider than no ink on tumor are needed. (Level of evidence: multiple randomized trials and meta-analysis.)
Should unfavorable biologic subtypes (such as triple-negative breast cancers) require wider margins (than no ink on tumor)?
Recommendation: Margins wider than no ink on tumor are not indicated based on biologic subtype. (Level of evidence: multiple retrospective studies.)
Should margin width be taken into consideration when determining whole-breast radiation delivery techniques?
Recommendation: The choice of whole-breast radiation delivery technique, fractionation, and boost dose should not be dependent on margin width. (Level of evidence: retrospective studies.)
Is the presence of lobular carcinoma in situ at the margin an indication for reexcision? Do invasive lobular carcinomas require a wider margin (than no ink on tumor)? What is the significance of pleomorphic lobular carcinoma in situ at the margin?
Recommendation: Wider negative margins than no ink on tumor are not indicated for invasive lobular cancer. Classic lobular carcinoma in situ at the margin is not an indication for reexcision. The significance of pleomorphic lobular carcinoma in situ at the margin is uncertain. (Level of evidence: retrospective studies.)
Should increased margin widths be considered for patients of young age (≤ 40 years)?
Recommendation: Young age (≤ 40 years) is associated with both increased ipsilateral breast tumor recurrence after breast-conserving therapy and increased local relapse on the chest wall after mastectomy and is also more frequently associated with adverse biologic and pathologic features. There is no evidence that increased margin width nullifies the increased risk of ipsilateral breast tumor recurrence in young patients. (Level of evidence: secondary data from prospective randomized trials and retrospective studies.)
What is the significance of an extensive intraductal component in the tumor specimen, and how does this affect margin width?
Recommendation: An extensive intraductal component identifies patients who may have a large residual ductal carcinoma in situ burden after lumpectomy. There is no evidence of an association between increased risk of ipsilateral breast tumor recurrence when margins are negative. (Level of evidence: retrospective studies.) ■
Disclosure: For full disclosures of the study authors, visit jco.ascopubs.org.
Reference
1. Moran MS, Schnitt SJ, Giuliano AE, et al: Society of Surgical Oncology–American Society for Radiation Oncology Consensus Guideline on Margins for Breast-Conserving Surgery With Whole-Breast Irradiation in Stages I and II Invasive Breast Cancer. Ann Surg Oncol. February 10, 2014 (early release online); Int J Radiat Oncol Biol Phys 88:553-564, 2014; J Clin Oncol. February 10, 2014 (early release online).