In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
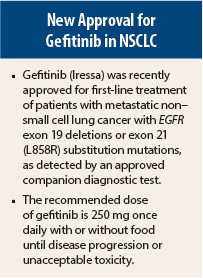
On July 13, 2015, gefitinib (Iressa) was approved for first-line treatment of patients with metastatic non–small cell lung cancer (NSCLC) with epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 (L858R) substitution mutations as detected by a U.S. Food and Drug Administration–approved test.1,2 The approval of gefitinib occurred concomitantly with a labeling expansion of the therascreen EGFR RGQ PCR Kit (Qiagen), a companion diagnostic test for patient selection.
Supporting Efficacy Data
Approval was based on the objective response rate in a multicenter single-arm trial in which 106 treatment-naive patients with metastatic EGFR-mutant NSCLC received gefitinib at 250 mg daily. Patients had a median age of 65 years (25% ≥ 75 years, 49% < 65 years), 100% were white, 71% were female, 64% were never-smokers, 93% had a World Health Organization performance status of 0 or 1, and 97% had adenocarcinoma histology (97%).
On blinded independent central review, the response rate was 50% (95% confidence interval [CI] = 41%–59%) with a median duration of response of 6.0 months. The investigator-determined response rate was 70% (95% CI = 61%–78%), with a median duration of response of 8.3 months.
The efficacy results are supported by an exploratory analysis of outcome in a subset of 186 of 1,217 patients in a randomized open-label trial of first-line gefitinib at 250 mg vs up to six cycles of carboplatin/paclitaxel in EGFR-mutant metastatic NSCLC. Patients in this subset had a median age of 59 years (7% ≥ 75 years, 70% < 65 years), 100% were Asian, 83% were female, 96% were never-smokers, 94% had a WHO performance status of 0 or 1, and 100% had adenocarcinoma histology.
As assessed by blinded independent central review, median progression-free survival in this subset analysis was 10.9 months in 88 gefitinib recipients vs 7.4 months in 98 carboplatin/paclitaxel recipients (hazard ratio = 0.54, 95% CI = 0.38–0.79). The objective response rate was 67% in gefitinib patients, with a median duration of response of 9.6 months, vs 41% in carboplatin/paclitaxel patients, with a median duration of response of 5.5 months.
How It Works
Activating EGFR mutations—eg, exon 19 deletion and exon 21 point mutation L858R—in NSCLC cells have been found to promote tumor cell growth, inhibit apoptosis, upregulate angiogenic factors, and promote metastasis. Gefitinib is a reversible inhibitor of the kinase activity of wild-type and activating mutations of EGFR, with prevention of autophosphorylation of tyrosine residues associated with the receptor resulting in inhibition of downstream signaling and EGFR-dependent proliferation.
The binding affinity of gefitinib for EGFR exon 19 deletion or exon 21 point mutation L858R mutations is higher than that for wild-type EGFR. Gefitinib also inhibits insulin-like growth factor– and platelet-derived growth factor–mediated signaling at clinically relevant concentrations.
How It Is Given
The recommended dose of gefitinib is 250 mg once daily with or without food until disease progression or unacceptable toxicity. Gefitinib should be withheld for up to 14 days for acute onset or worsening of pulmonary symptoms (dyspnea, cough, fever), grade ≥ 2 alanine transaminase (ALT) or aspartate transaminase (AST) elevation, grade ≥ 3 diarrhea, signs or symptoms of severe or worsening ocular disorders including keratitis, and grade ≥ 3 skin reactions. Treatment can be resumed when the adverse reaction fully resolves or improves to grade 1. Gefitinib should be permanently discontinued for confirmed interstitial lung disease, severe hepatic impairment, gastrointestinal perforation, and persistent ulcerative keratitis.
The gefitinib dose can be increased to 500 mg daily in the absence of severe adverse drug reactions when used concomitantly with strong CYP3A4 inducers (eg, rifampicin, phenytoin, tricyclic antidepressants), with treatment being resumed at 250 mg 7 days after discontinuation of the strong CYP3A4 inducer. Strong CYP3A4 inhibitors (eg, ketoconazole, itraconazole) increase gefitinib concentrations, warranting heightened monitoring for adverse reactions with concomitant use.
Drugs that elevate gastric pH can reduce gefitinib levels. Gefitinib should be given 12 hours after the last dose or 12 hours before the next dose of a proton pump inhibitor and 6 hours before or after an H2-receptor antagonist or antacid.
International normalized ratio (INR) elevations and hemorrhage have been reported in patients taking warfarin during gefitinib treatment. Patients taking warfarin should be monitored regularly for changes in prothrombin time or INR.
Safety Profile
Safety data for gefitinib are from 2,462 patients with NSCLC who received monotherapy at 250 mg daily in three randomized clinical trials. Patients with a history of interstitial lung disease, drug-induced interstitial disease, radiation pneumonitis that required steroid treatment, or any evidence of clinically active interstitial lung disease were excluded from these trials.
Data on common adverse events are from one randomized clinical trial in which 1,126 patients received gefitinib at 250 mg daily and 562 patients received placebo as second- or third-line treatment for metastatic NSCLC. The most common adverse events of any grade occurring more frequently in the gefitinib group were skin reactions (47% vs 17%), diarrhea (29% vs 10%), decreased appetite (17% vs 14%), and vomiting (14% vs 10%); the most common grade 3 or 4 adverse events were diarrhea (3% vs 1%), decreased appetite (2.3% vs 2.0%), and skin reactions (2.0% vs 0.4%).
The most common laboratory abnormalities of any grade occurring more frequently in gefitinib recipients were increased ALT (38% vs 23%, grade 3 or 4 in 2.4% vs 1.4%), increased AST (40% vs 25%, grade 3 or 4 in 2.0% vs 1.3%), and proteinuria (35% vs 31%, grade 3 or 4 in 4.7% vs 3.3%). Approximately 5% of gefitinib patients and 2.3% of placebo patients discontinued treatment due to adverse events, with the most common reasons in gefitinib patients being nausea (0.5%), vomiting (0.5%), and diarrhea (0.4%). The most frequent fatal adverse events in gefitinib patients were respiratory failure (0.9%), pneumonia (0.8%), and pulmonary embolism (0.5%).
Serious and uncommon adverse drug reactions observed in the pooled population of NSCLC patients receiving gefitinib monotherapy included interstitial lung disease (1.3%), fatal hepatotoxicity (0.04%), and grade 3 ocular disorders (0.1%).
Gefitinib carries warnings/precautions for interstitial lung disease, hepatotoxicity, gastrointestinal perforation, ocular disorders including keratitis, bullous and exfoliative skin disorders, and embryofetal toxicity. Patients receiving gefitinib should undergo periodic liver function testing. Women should not breast-feed during treatment. ■
References
1. U.S. Food and Drug Administration: Gefitinib (Iressa). Available at http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm454692.htm. Accessed July 28, 2015.
2. Iressa (gefitinib) tablets prescribing information, AstraZeneca, July 2015. Available at http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/206995s000lbl.pdf. Accessed July 28, 2015.