Two early-phase studies have shown that the novel epidermal growth factor receptor (EGFR) inhibitors rociletinib and AZD9291 exhibit high activity in non–small cell lung cancer (NSCLC) patients with the EGFR T790M mutation who had progressed on prior EGFR inhibitor therapy.1,2 The T790M mutation confers resistance to current EGFR inhibitors. The novel inhibitors are also active in disease with sensitizing EGFR mutations, and both also produced responses in T790M-negative patients who had previously received EGFR inhibitor therapy.
Both rociletinib and AZD9291 have been granted Breakthrough Therapy status by the U.S. Food and Drug Administration, and both agents continue to be studied in ongoing clinical trials.
Rociletinib Study
In a phase I/II study1 reported in The New England Journal of Medicine by Lecia V. Sequist, MD, MPH, of Massachusetts General Hospital and Harvard Medical School, and colleagues, 92 evaluable patients with advanced EGFR-mutant NSCLC that had progressed on treatment with an EGFR inhibitor were treated with a free-base form of rociletinib (first group of enrolled patients) at a dose of 900 mg twice daily (10 with centrally confirmed presence or absence of T790M mutation) or a hydrogen bromide salt form at doses of 500 mg twice daily to 1,000 mg twice daily (all remaining patients; 53 with centrally confirmed presence or absence of T790M mutation).
Responses
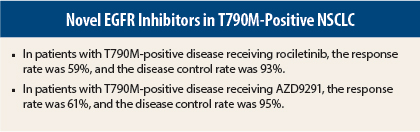
A total of 83 patients were evaluable for response. Among 46 patients with centrally confirmed T790M-positive tumors, 59% (95% confidence interval [CI] = 45%–73%) had a partial response, and 35% had stable disease (disease control rate = 93%). Response rates were similar in patients with deletion 19 or L858R EGFR mutations.
At the time of analysis, estimated median progression-free survival was 13.1 months (95% CI = 5.4–13.1 months), with data censored for 82% of patients. Among 17 patients with T790M-negative tumors on central testing, the response rate was 29% (95% CI = 8%–51%), and 29% had stable disease (disease control rate = 59%). Estimated median progression-free survival in these patients was 5.6 months (95% CI = 1.3 months to not reached). Among 20 patients whose tumors were not assessable for T790M mutation, the response rate was 15%.
Safety
No maximum tolerated dose of rociletinib was identified. The most common dose-limiting adverse event was hyperglycemia. Among 92 patients receiving therapeutic doses of rociletinib, the most common treatment-related adverse events of any grade were hyperglycemia (47%), nausea (35%), fatigue (24%), and diarrhea (22%); QTc prolongation occurred in 12%.
The most common grade 3 adverse events were hyperglycemia (22%) and QTc prolongation (5%). Glucose-lowering treatment was required in 38% of patients. Patients with grade 3 QTc prolongation were asymptomatic and managed by dose reduction. No acneiform rash was observed; one patient had maculopapular rash. Overall, 48% of patients had dose reduction.
The investigators concluded: “Rociletinib was active in patients with EGFR-mutated NSCLC associated with the T790M resistance mutation.”
AZD9291 Study
In a phase I study2 of predominantly Asian patients reported in The New England Journal of Medicine by Pasi A. Jänne, MD, of Dana-Farber Cancer Institute, and colleagues, 253 evaluable patients with advanced disease who had disease progression after prior EGFR inhibitor therapy received AZD9291 at daily dose levels of 20 mg to 240 mg.
Responses
Among 239 patients evaluable for response, 51% (95% CI = 45%–58%) responded (one complete response), and 33% had stable disease (disease control rate = 84%). Response rates were 50% among 150 Asian patients and 54% among 89 non-Asian patients. Response rates were similar at each of the AZD9291 dose levels.
Among 127 evaluable patients with centrally confirmed T790M mutation, the response rate was 61% (95% CI = 52%–70%), and the disease control rate was 95%. Among 61 evaluable patients with no T790M mutation on central testing, the response rate was 21% (95% CI = 12%–34%), and the disease control rate was 61%.
Median progression-free survival was 9.6 months (95% CI = 8.3 months to not reached) in T790M-positive patients and 2.8 months (95% CI = 2.1–4.3 months) in T790M-negative patients.
Safety
No maximum tolerated dose was identified. Among 253 patients in the safety analysis, the most common adverse events of any grade were diarrhea (47%), rash (40%), nausea (22%), and decreased appetite (21%); diarrhea and rash appeared to be dose-dependent.
Adverse events of grade ≥ 3 occurred in 32% of patients. Adverse events led to dose reduction in 7% and treatment discontinuation in 6%. Six patients (2%) had pneumonitis-like events, with all of them discontinuing treatment. QTc prolongation occurred in 4% of patients, and hyperglycemia occurred in 2%, with no dose reduction or discontinuation in any of these patients. There were no significant differences in the severity or frequency of adverse events between Asian and non-Asian patients.
The investigators concluded: “AZD9291 was highly active in patients with lung cancer with the EGFR T790M mutation who had had disease progression during prior therapy with EGFR tyrosine kinase inhibitors.” ■
Disclosure: The rociletinib study was funded by Clovis Oncology. The AZD9291 study was funded by AstraZeneca. For full disclosures of the study authors, visit www.nejm.org.
References
1. Sequist LV, et al: Rociletinib in EGFR-mutated non-small-cell lung cancer. N Engl J Med 372:1700-1709, 2015.
2. Jänne PA, et al: AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med 372:1689-1699, 2015.