In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
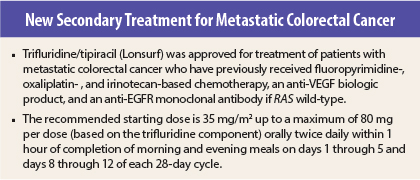
On September 22, 2015, trifluridine/tipiracil (Lonsurf) was approved for treatment of patients with metastatic colorectal cancer who have previously received fluoropyrimidine-, oxaliplatin- , and irinotecan-based chemotherapy, an anti-VEGF (vascular endothelial growth factor) biologic product, and an anti-EGFR (epidermal growth factor receptor) monoclonal antibody if RAS wild-type.1,2
Supporting Efficacy Data
Approval was based on findings in a double-blind phase III trial in which 800 patients with previously treated metastatic colorectal cancer were randomized 2:1 to receive trifluridine/tipiracil (n = 534) or placebo (n = 266) plus best supportive care.2,3 Patients received trifluridine/tipiracil 35 mg/m2 (based on trifluridine component) or placebo orally twice daily on days 1 to 5 and 8 to 12 of each 28-day cycle until disease progression or unacceptable toxicity. Eligibility requirements included Eastern Cooperative Oncology Group performance status of 0 or 1, absence of brain metastasis, and absence of ascites requiring drainage in the past 4 weeks.
Patients had a median age of 63 years, 61% were male, 58% were white and 35% were Asian, the primary disease site was the colon in 62% and the rectum in 38%, and KRAS status was wild-type in 49% and mutant in 51%. All patients received prior treatment with fluoropyrimidine-, oxaliplatin-, and irinotecan-based chemotherapy, all except one received bevacizumab (Avastin), and all except two with KRAS wild-type tumors received panitumumab (Vectibix) or cetuximab (Erbitux).
Median overall survival was 7.1 months (95% confidence interval [CI] = 6.5–7.8 months) in the trifluridine/tipiracil group vs 5.3 months (95% CI = 4.3–6.0 months) in the placebo group (hazard ratio [HR] = 0.68, P < .001). Progression-free survival was also significantly prolonged in the trifluridine/tipiracil group (HR = 0.47, P < .001).
How It Works
The agent consists of the thymidine-based nucleoside analog trifluridine and the thymidine phosphorylase inhibitor tipiracil (molar ratio = 1:0.5; weight ratio = 1:0.471). Tipiracil acts to increase trifluridine exposure by inhibiting its metabolism by thymidine phosphorylase. After uptake into cancer cells, trifluridine is incorporated into DNA, interfering with DNA synthesis and inhibiting cell proliferation. Trifluridine/tipiracil exhibited antitumor activity against KRAS wild-type and mutant colorectal cancer xenografts in mice.
How It Is Used
The recommended starting dose is 35 mg/m2 up to a maximum of 80 mg per dose (based on the trifluridine component) orally twice daily within 1 hour of completion of morning and evening meals on days 1 through 5 and days 8 through 12 of each 28-day cycle until disease progression or unacceptable toxicity. Doses should be rounded to the nearest 5-mg increment.
Complete blood cell counts must be obtained prior to and on day 15 of each cycle. A treatment cycle should not be started until absolute neutrophil count (ANC) is ≥ 1,500/mm3 or febrile neutropenia is resolved, platelet count is ≥ 75,000/mm3, and grade 3 or 4 nonhematologic adverse reactions are resolved to grade 0 or 1. Within a treatment cycle, the drug should be withheld for an ANC < 500/mm3 or febrile neutropenia, platelet count < 50,000/mm3, or grade 3 or 4 nonhematologic adverse reactions.
After recovery, treatment can be resumed after reducing the dose by 5 mg/m2 per dose from the previous dose level if the patient experiences febrile neutropenia, uncomplicated grade 4 neutropenia or thrombocytopenia that delays the start of the next cycle by > 1 week, or nonhematologic grade 3 or 4 adverse reactions (except for grade 3 nausea and/or vomiting controlled by antiemetic therapy or grade 3 diarrhea responsive to antidiarrheal medication). A maximum of three dose reductions are permitted to a minimum dose of 20 mg/m2 twice daily. The dose should not be increased after it has been reduced.
Trifluridine and tipiracil are not metabolized by CYP450 enzymes and do not inhibit or induce CYP450 enzymes or inhibit or act as a substrate for uptake and efflux transporters.
No dose modification is recommended in patients with mild hepatic impairment. No patients with moderate or severe impairment were enrolled in the phase III study. No adjustment is recommended for patients with mild or moderate renal impairment.
However, patients in the phase III trial with moderate impairment had a higher rate of grade ≥ 3 adverse events, serious adverse events, and dose delays and reductions compared with patients with normal renal function or mild impairment. Thus, patients with moderate renal impairment may require dose modification for increased toxicity. No patients with severe renal impairment were enrolled in the phase III study.
Safety Profile
In the phase III trial, the most common adverse events of any grade occurring > 2% more frequently in the trifluridine/tipiracil group were anemia (77% vs 33%), neutropenia (67% vs 1%), asthenia/fatigue (52% vs 35%), nausea (48% vs 24%), thrombocytopenia (42% vs 8%), decreased appetite (39% vs 29%), diarrhea (32% vs 12%), vomiting (28% vs 14%), and abdominal pain (21% vs 18%). The most common grade 3 or 4 adverse events were neutropenia (38% vs 0%), anemia (18% vs 3%), asthenia/fatigue (7% vs 9%), thrombocytopenia (5% vs <1%), and decreased appetite (4% vs 5%). Infections occurred in 27% vs 15% of patients. Pulmonary embolism was observed in 2% vs 0%. Grade 3 or 4 neutropenia and thrombocytopenia and grade 3 anemia were more common in patients aged older than 65 years. As noted, patients with moderate renal impairment had increased rates of adverse events and dose modifications.
Adverse events led to drug discontinuation in 3.6% of trifluridine/tipiracil patients and to dose reduction in 13.7%; the most common causes of dose reduction were neutropenia, anemia, febrile neutropenia, fatigue, and diarrhea.
Trifluridine/tipiracil carries warnings/precautions for severe myelosuppression and embryo-fetal toxicity. Women should not breastfeed while receiving the drug. ■
References
1. U.S. Food and Drug Administration: Approved drugs. Trifluridine/tipiracil. Available at http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm463743.htm. October 7, 2015.
2. Lonsurf (trifluridine and tipiracil) tablets prescribing information, Taiho Oncology, Inc, September 2015. Available at https://www.taihooncology.com/us/prescribing-information.pdf. October 7, 2015.
3. Mayer RJ, Van Cutsem E, Falcone A, et al: Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med 372:1909-1919, 2015.
Report Adverse Events
Health-care professionals should report all serious adverse events suspected to be associated with the use of any medicine or device to FDA’s MedWatch Reporting System by completing a form online at http://www.fda.gov/medwatch/report.htm, by faxing (1-800-FDA-0178), by mailing the postage-paid address form provided online, or by telephone (1-800-FDA-1088).