In a study reported in The New England Journal of Medicine, Peled et al found that intestinal microbiota from patients undergoing allogeneic hematopoietic cell transplantation at four centers showed patterns of disruption characterized by loss of diversity and domination by a single taxon. Lower diversity was associated with significantly poorer overall survival.
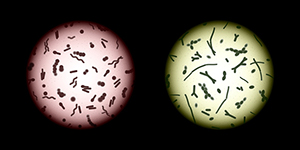
Photo credit: Getty
Study Details
The study involved identification of microbiota composition of 8,767 fecal samples from 1,362 patients undergoing allogeneic hematopoietic cell transplantation at Memorial Sloan Kettering Cancer Center (MSK; cohort 1) and at Duke University Medical Center; the University Medical Center, University Hospital Regensburg, Germany; and Hokkaido University, Sapporo, Japan (cohort 2). Stool samples were obtained between day 7 and 21 of the transplantation period. The median diversity value of microbiota at MSK (2.64) was used to distinguish between higher-diversity (> 2.64) and lower-diversity microbiota in both cohorts.
Key Findings
Loss of diversity was observed in patients from all four centers during the course of the transplantation period (P < .001 for each center), with domination by a single taxon being observed.
Among patients at MSK (cohort 1), death occurred in 104 of 354 patients in the higher-diversity group vs 136 of 350 patients in the lower-diversity group (hazard ratio [HR] = 0.75, 95% confidence interval [CI] = 0.58–0.96). The association remained significant in multivariate analysis adjusting for age, intensity of conditioning regimen, graft source, and the hematopoietic cell transplantation comorbidity index (adjusted HR = 0.71, 95% CI = 0.55–0.92). In cohort 2, there were 18 deaths among 87 patients in the higher-diversity group vs 35 deaths among 92 patients in the lower-diversity group (adjusted HR = 0.49, 95% CI = 0.27–0.90).
Subgroup analyses indicated an association between lower diversity and higher risk of transplantation-related death and death attributable to graft-vs-host disease. In cohort 1, there were 30 transplantation-related deaths among 244 patients in the higher-diversity group vs 46 among 184 patients in the lower-diversity group among recipients of unmodified grafts (HR = 0.49, 95% CI = 0.31–0.77); no significant association was observed among recipients of T cell–depleted grafts. Among recipients of unmodified grafts, there were 17 graft-vs-host disease–related deaths among 244 patients in the higher-diversity group vs 26 among 184 patients in the lower-diversity group (HR = 0.49, 95% CI = 0.26–0.90).
In cohort 1, higher diversity in pretransplantation samples (with diversity assessed as a continuous variable) was associated with improved survival (adjusted HR = 0.41, 95% CI = 0.24–0.71). There was a weak correlation between baseline and transplantation period diversity (r = 0.22). No association between baseline diversity and survival was observed in cohort 2.
The investigators concluded, “Patterns of microbiota disruption during allogeneic hematopoietic cell transplantation were similar across transplantation centers and geographic locations; patterns were characterized by loss of diversity and domination by single taxa. Higher diversity of intestinal microbiota at the time of neutrophil engraftment was associated with lower mortality.”
Disclosure: The study was funded by the National Cancer Institute and others. For full disclosures of the study authors, visit nejm.org.

